Introduction
The purpose of this leaflet is to provide you with information about Achilles tendinopathy and ways to manage this condition. Most people experience a gradual improvement in symptoms by following this advice.
What is Achilles tendinopathy?
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel bone. It is made up of bundles of a very strong material called collagen. The Achilles tendon pulls on the heel and points the foot down. This movement is used to push off the ground while running and walking. Tendinopathy occurs when the tendon is not able to adapt to the loads placed on it. This abnormal load can cause pain, swelling and stiffness of the tendon.
What are the symptoms?
People often describe pain around their heel. Sometimes pain can occur in the mid portion or at the lower part of the tendon. Pain is usually worse during or after activity. Some people experience stiffness in the morning or after periods of rest. The tendon may also become thickened around the painful area.
What are the causes?
The exact cause is not fully understood. There are several potential factors that can lead to Achilles tendinopathy. Some of these factors cannot be controlled e.g. age, genetics and body alignment. The positive news is usually these factors only increase the risk of developing tendon problem slightly.
There are, however, some factors that we can change to reduce the risk of a tendon problem.
- Activity/overuse. Increasing the loading on the tendon rapidly. This is often caused by doing too much walking, running or jumping without adequate preparation.
- Obesity. Excess weight increases load on your tendons, obesity may also increase risk due to biochemical mechanisms.
- Elevated cholesterol. High cholesterol is a risk factor for tendon problems.
- Hormonal changes. Women are more susceptible around the menopause. This may be due to reduced estrogen levels at this time.
- Muscle weakness. Weak muscles are less able to protect the tendon. This can increase loads on the tendon and the risk of tendinopathy.
- Biomechanics: The way that you move as well as your joint flexibility may place increased loads on your tendons and increase injury risk.
The role of load and a healthy tendon
How much load is placed through your tendon has a major effect on keeping your tendon healthy and pain free. Too much load is not helpful, for example running long distances without building up to those distances over a period of months before hand. Too little load also is not helpful, for example being inactive (Figure 1).
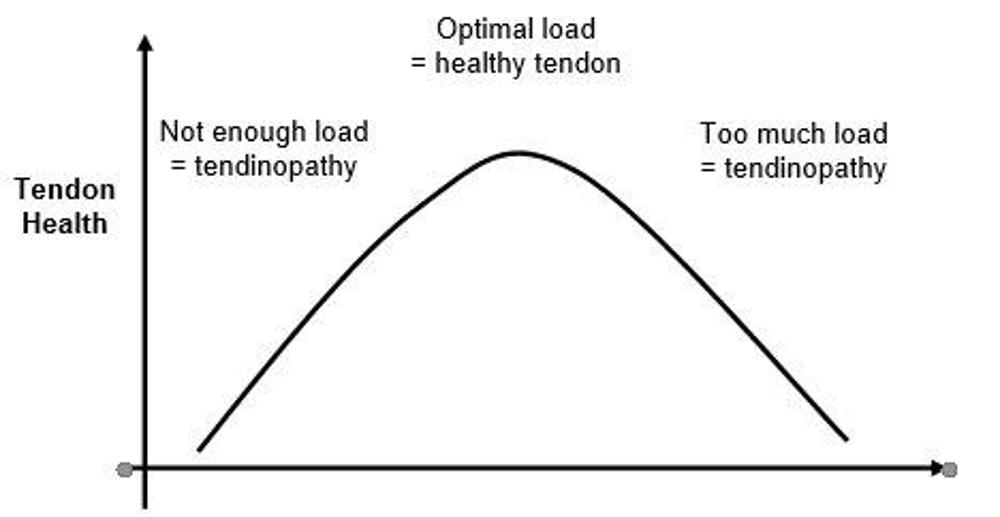
Figure 1: Tendon health and loading
The goal of this home based rehabilitation programme is to gradually load your tendon over a period of time. This will allow you to be able to comfortably manage the tasks and activities that you enjoy doing.
Should I have an x-ray or scans?
This condition is usually diagnosed by a clinical examination and the symptoms you report. It is not necessary to have an x-ray or scan of your tendon to diagnose this condition. A healthcare professional can advise you if you require further investigations. If you have already had a scan, there are some important messages you should be aware of regarding the results of scans.
- Pathology in the tendon is common in people without pain
- Even with very severe pathology your pain can improve
- Painful and pathological tendons hardly ever tear suddenly.
What is the prognosis?
Most people will see some improvement within 3 to 6 months. Some people can experience mild and ongoing symptoms for several months.
Do not panic if you have a flare-up of your pain as small setbacks during the healing period are quite common. It may take up to 6 to 12 months for symptoms to fully settle. Occasionally symptoms may recur.
Self-care, advice and exercise should help you cope with your symptoms and aid recovery.
Treatment
What can I do myself to help?
Advice to help improve symptoms.
- Avoid or decrease the activities which cause your pain.
- Strengthen the muscles in your legs.
- Try to keep active and stay at work, even if you have to modify your duties.
- Apply an ice pack for 5 to 10 minutes two to three times a day to manage pain. Make sure you place a damp towel between the ice and your skin to prevent an ice burn. Further information can be found on the NHS Inform website nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints/guidelines/price-guidelines.
- Using painkillers to provide short term relief. Discuss these with your pharmacist, General Practitioner (GP) or healthcare practitioner.
Home rehabilitation programme for management of Achilles tendinopathy
The main principles when gradually rehabilitating your Achilles tendon are below.
- Alter the load through the tendon to a more manageable level
- Increase the load tolerance of the tendon and muscles
- Increase the load tolerance of the other leg muscles.
How can physiotherapy help?
It is very important that you have an active role in the management of your condition and work to improve your condition. Working with your physiotherapist and through this leaflet can help you manage load through the tendon in a more appropriate manner. It will also help build the tolerance of the muscles and tendons in your leg.
Load management
It is important to try to reduce some of the factors that irritate your symptoms. These may include reducing the amount of walking or running you would normally do, avoid calf stretches if they are painful and avoid flat heeled shoes or walking barefooted. You may even wish to consider wearing a small heel wedge in your shoe, as this may reduce your symptoms while walking or running.
Exercises
It is acceptable to experience discomfort while doing these exercises. This is normal and does not cause any damage. Discomfort, however, should be at a level you consider to be manageable and should settle within 24hrs. It is advised that you gradually progress through these exercises over a period of at least 12 weeks to see meaningful improvement in your symptoms. During this period, you might experience a slight increase in pain, this is called a flare up. If this happens let your symptoms settle, then return to the exercises at a lower level. The exercises should be challenging, but manageable.
Rehabilitation exercises
How often should I do these exercises?
Stretching
There is no exact stretching time that works for everyone. Current evidence suggests stretching for 30 to 60 seconds in total may be optimal. This could be one or two sets of 30 second holds or three sets of 20 seconds.
It is, however, best to start with one or two stretches held for 10 seconds or so and gradually build this up to between 30 and 60 seconds. Stretching can feel uncomfortable, but should not feel painful during or after the exercise.
Rehabilitation exercises
Try to do these exercises once a day on the majority of days. It is important to have rest days, especially if you are not used to exercising regularly. It is acceptable to break the exercises into groups and complete these at different times in the day.
Start with one set of 5 to 10 repetitions. As the exercise becomes easier you can either gradually increase the repetitions or add another set of exercises. A total of 45 repetitions would be a maximal effort i.e. 3 sets of 15 repetitions. Take a rest of up to a minute between each set. Ideally the muscle(s) you are exercising should begin to feel fatigued by the end of the exercise however you should not be straining. It is normal to have some discomfort during exercises as long as it’s acceptable to you.
As you increase the repetition of exercises you should try to have a rest day after each exercise day to allow your muscles to recover.

1. Seated Heel Raise and Hold
Sitting in a chair.
Weight evenly on both feet, slowly push up onto your tip toes, hold for 10 seconds and then slowly lower to starting position.

2. Standing Heel Raise and Hold
Stand using the back of a chair or kitchen top for balance.
Weight evenly on both feet, slowly push up onto your tip toes and then slowly lower to starting position.
You may need to put more weight through your uninjured leg to start with, but over the next few weeks gradually try to put more and more weight through the injured leg as the muscles become stronger.

3. Heel raises with knees bent (Soleus Strengthening
Stand with your feet apart.
Bend your knees and then slowly lift your heels.

4. Gastroc-nemius Stretch
Stand in a walking position with the leg to be stretched straight behind you and the other leg bent in front of you. Take support from a wall or chair.
Lean your body forwards and down until you feel the stretching in the calf of the straight leg. Stretch the other leg.

5. Soleus Stretch
Stand in a walking position with the leg to be stretched behind you. Hold on to a support.
Bend the leg to be stretched and let the weight of your body stretch your calf without lifting the heel off the floor.

6. Through Range Quadriceps
Sit in a chair, tighten your thigh muscles and straighten your knee.
Hold for 5 to 10 seconds and slowly lower to starting position.

7. Standing Hamstring Curls
Stand. Put a small weight around your ankle. Hold onto a support and bring one leg slightly backwards.
Bend your knee and lift your foot off the floor. Hold 5 to 10 seconds.

8. Hip Abductor Strengthening
Lie on your side, with the lower leg bent and the upper leg straight.
Slowly lift the upper leg straight up with ankle flexed. Return to the starting position.
Progression Exercises:
Criteria for Progression.
- Minimal or no pain
- Minimal or no swelling
- Good range of movement
- Minimal symptoms with previous exercises.
Repeat the previous exercises and add the following:


1. Hip Hinge
Stand tall holding a stick or golf club or umbrella with both hands. With almost straight knees, tilt your trunk forwards and push your bottom backwards until you can feel a pull in the back of your thighs.
Thrust hips forward and stand tall to return to starting position and repeat. Keep the stick close to your body throughout. This can be made more challenging by exchanging the stick for something heavier like a full shopping bag or kettlebell if available.


2. Bridging
Lie on your back, with knees bent and feet hip-width apart.
Squeeze your buttocks, push your heels into the floor or bed and drive your bottom up, hold and slowly lower to starting position.

3. Box Squat
Sitting with your arms crossed.
Stand up and then sit down slowly on a chair. (This can be made easier or more difficult by changing the height of the).


4. Single Leg Heel Raise
Stand on one leg on a step or bottom stair with your heel over the edge.
Use the handrail for balance. Let your heel drop downwards.
Slowly push up onto your tip toes, pause and then slowly lower to the starting position.

5. Jogging on the Spot
If you are someone who enjoys running, it is recommended that you start off jogging on the spot for a short period of time (e.g. 5 minutes). If too easy (no pain or limp) then progress to light jogging.
It is recommended that you do this in a graduated manner. The NHS ‘Couch to 5K’ running programme can be a useful way of doing this
Getting back to normal
Returning to activities of daily living
There are no specific timeframes regarding when you can return to activities of daily living. It is advised that you aim to gradually build up the exercises in this leaflet and then gradually return to activities as able. It is advised that you use the same guidelines regarding discomfort as for the exercises, i.e. discomfort should be at a level you consider to be manageable and should settle within 24hrs.
Guidance for returning to work
Research suggests that staying active and keeping moving as pain allows, will help you get better sooner. Getting back to work helps most people with back pain. If you are ‘signed-off’ work, time frames for returning to work will depend on the type of work you do and a healthcare professional can advise on this. It is advised you communicate regularly with your employer to facilitate a safe and timely return to work.
Useful information
NHS Inform
www.nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints
NHS Inform – How to Apply ICE
https://www.nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints/
NHS Fitness Studio – Couch to 5k
www.nhs.uk/live-well/exercise/running-and-aerobic-exercises/get-running-with-couch-to-5k/
The Chartered Society of Physiotherapy
www.csp.org.uk/conditions/managing-your-bone-joint-or-muscle-pain
Worries or concerns
Should you have any worries or concerns, please contact your Physiotherapist, Podiatrist or GP during working hours or contact NHS24 on 111 out of working hours.
If you continue to experience problems then you should consult a healthcare professional.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.





