Introduction
Most back pain cases settle quickly but can be very painful initially. This may require modification of your everyday activities for a couple of days.
Resting longer than this does not help and may do more harm than good. It is essential to keep moving. The sooner you return to normal activities, the sooner your back will start feeling better.
What actually causes ‘non-specific’ spinal pain?
The honest answer is that we do not really know. We think there may be several reasons for ‘Non-Specific’ Spinal Pain. 1) Either the tissues becomes stretched beyond their normal limit. Like an elastic band that has been overstretched and does not quite go back to its original shape. This may be the result of a specific injury or repetitive factors.
What are the symptoms?
These vary from person to person. People may experience:
- Back or buttock pain
- Muscle spasm
- Reduced back movements
Sciatica
Back pain may sometimes be accompanied by a pain that travels down the buttock into the leg. This is called sciatica, usually caused by a slipped disc irritating a nearby nerve. Patients with sciatica may also notice areas of numbness or a pins and needles sensation in the affected leg. They may see weakness in specific muscles in their leg. Sciatica will usually improve over 8 to 10 weeks and does not require an urgent MRI scan or x-ray at this stage.
How can I help myself?
- Stay active - regular exercise can help to keep your back strong.
- If you have to go to bed, try to start moving again after two days and gradually increase your activity daily. This can cause discomfort for a short time and is to be expected, but it is important to keep trying.
- Try exercises and stretches for back pain in this leaflet.
- Take simple painkillers such as paracetamol and ibuprofen to help manage this pain. Please don’t wait until the pain becomes uncontrollable before you take them.
- Use heat (such as a hot water bottle or wheat bag) or cold (a bag of frozen peas wrapped in a wet towel) to give short-term relief. This is in addition to your medication.
- Do not stay in one position for longer than 20 to 30 minutes. It is important to keep moving around. Prolonged sitting, especially in a low soft armchair, can worsen the pain.
When should I make an appointment with my GP?
If symptoms have not improved after four weeks, please make a non-urgent appointment with your GP or Nurse Practitioner. In addition, if you notice non-intentional weight loss or back pain, which is worse at night, you should make an appointment with your GP.
When should I return to A&E?
If any of the following occur in the context of back pain, then you should return immediately to A&E at the Victoria Hospital, Kirkcaldy for review to exclude serious spinal conditions:
Warning Signs
If you have severe pain which is getting worse over several weeks, or if you are unwell with back pain, you should consult your doctor. The following symptoms are very rare, but if you suddenly develop any of them, you should consult a doctor straightaway.
- Back pain with Fever (temperature) of 38˚C or more.
Cauda Equina Syndrome Warning Signs
Many patients have a combination of back pain, leg pain, leg numbness and weakness. These symptoms can be distressing, but do not necessarily require emergency medical attention.
A rare, but serious back condition, Cauda Equina Syndrome, can lead to permanent damage or disability and will need to be seen by an Emergency Specialist Spinal Team. Some warning signs of Cauda Equina Syndrome are as follows:
- Loss of feeling/pins and needles between your inner thighs or genitals
- Numbness in or around your back passage or buttocks
- Altered feeling when using toilet paper to wipe yourself
- Increasing difficulty when you try to urinate
- Increasing difficulty when you try to stop or control your flow of urine
- Loss of sensation when you pass urine
- Leaking urine or recent need to use pads
- Not knowing when your bladder is either full or empty
- Inability to stop a bowel movement or leaking
- Loss of sensation when you pass a bowel motion
- Change in ability to achieve an erection or ejaculate
- Loss of sensation in genitals during sexual intercourse
Any one or combination of these seek medical help immediately.
Exercises for the back
These exercises aim to help you move normally and safely.
How many times and how often?
- Start with 5 to 10 repetitions of each exercise.
- Add one or two repetitions more every few days or as pain allows.
- Try to exercise about three times a day.
- Be guided by your pain. If they cause increase or cause pain in the leg(s) then stop.

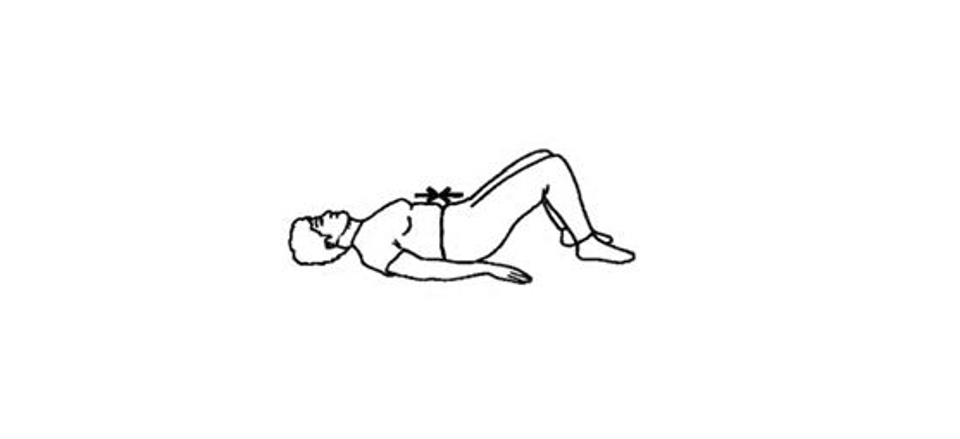
1. Lying on your back with knees together and bent. Slowly roll your knees from side to side, keeping your upper body still.
2. Lying on your back with knees bent and arms by your side. Tighten your stomach muscles and press the small of your back against the floor, letting your bottom rise. Hold for 5 seconds, and then relax.
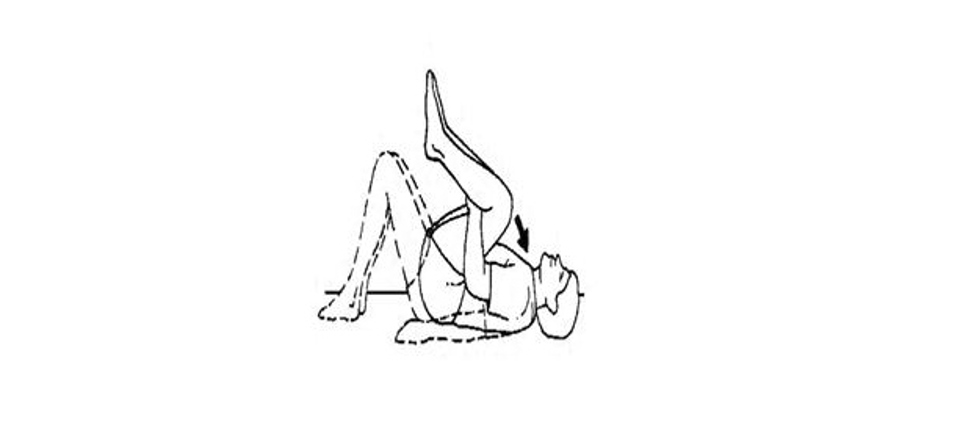
3. Lying with your knees bent and feet on the floor. Lift your knees towards your chest. Place your hands behind both knees and draw them towards your chest. Hold for 5 seconds, and then return your feet to the floor.
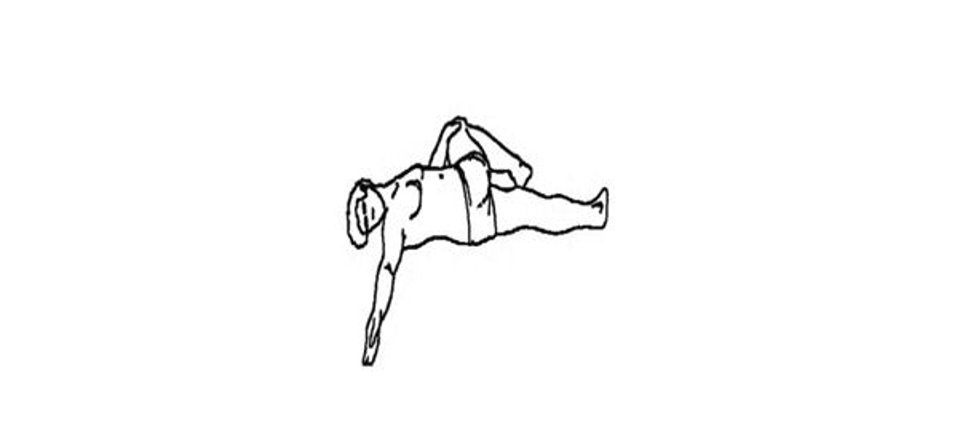
4. Lying on your back with one leg bent. Bring your bent knee over the other leg and push your knee against the floor with the opposite hand. Then reach with the other arm to the opposite side, looking in the same direction. You will feel the stretching in your lower back and bottom. Hold approx. 20 seconds and then back.
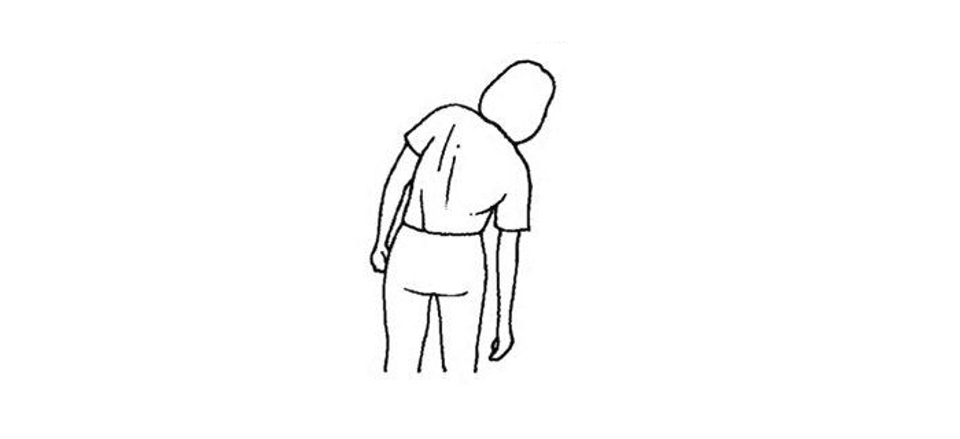
5. Bend sideways at the waist. Repeat three times to each side.
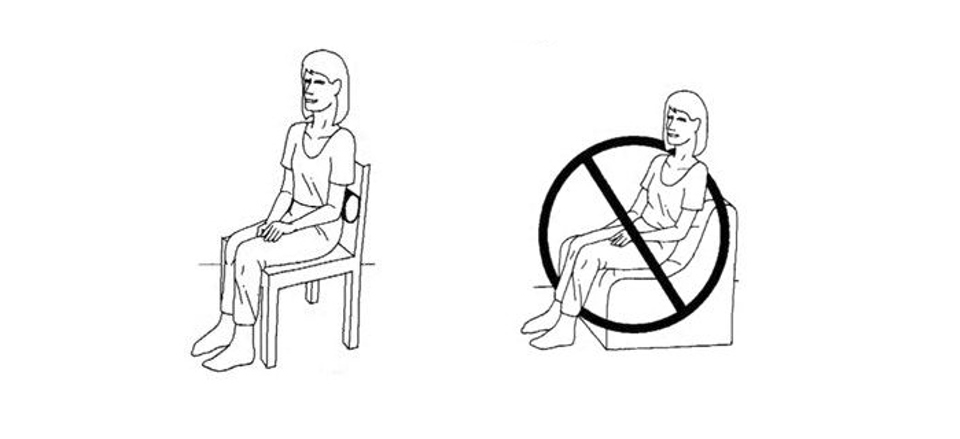
6. Try to avoid poor sitting posture. Sit with back support, and don't sit for long periods.
Pain relief and comfort
- You can take pain relief such as Paracetamol and Ibuprofen. Your local pharmacist can also advise.
Getting back to normal
If working you can self-certify for one week
Worries or concerns
Should you have any worries or concerns following discharge from the hospital, please contact your GP during working hours or contact NHS24 on 111 out of working hours.
If there is no improvement in your condition after 4 to 6 weeks, you should seek the advice of a healthcare professional. If your pain does not settle, you may be referred for further assessment and treatment as appropriate. In 9 out of 10 cases, pain resolves without specialist treatment.
Useful Information
NHS Inform – www.nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints
Chartered Society of Physiotherapy – www.csp.org.uk/conditions/managing-your-bone-joint-or-muscle-pain
For free and confidential advice about work call the Healthy Working Lives Advice line on 0800 019 2211 www.healthyworkinglives.com
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.




